In 2015, Improving Diagnosis in Health noted 5% of U.S. adults seeking outpatient care experienced diagnostic error.
A review of inpatient event reports indicates that diagnostic errors account for 6–17% of reported adverse events,1 and failure to respond to new, actionable information is a frequent cause of diagnostic error in both the outpatient and inpatient settings.
Closing the loop means that all mechanisms are in place to ensure that any patient data and information that may require action are delivered and communicated to the right individuals, at the right time, through the right mode, in order to allow for interpretation, critical review, reconciliation, initiation of action, acknowledgement, and appropriate documentation.2 Failure to close the loop on diagnostic test results is one example
of a failure to respond to actionable information.
Consider the following examples:
DELAYED DIAGNOSIS
A patient was seen for evaluation of testicular pain from possible testicular torsion. An ultrasound was performed. The initial verbal report stated that no torsion was seen. One week later, the final report noted a “suspicious mass,” with recommendations for the patient to follow up with a urologist. The report was signed by both the nurse practitioner and the physician.
Unfortunately, the patient was never informed, and returned seven months later complaining again of pain. A large testicular mass was discovered on physical examination.
This example shows multiple points of failure. First, the verbal report had not provided all the information. Second,despite the fact that the written report was signed, its recommendations were not acknowledged. Finally, no actions were taken—and as a result, the patient was not made aware of the “suspicious mass” for seven months.
Failing to close the loop on diagnostic testing is not a new problem. While the introduction of health information technology (IT) was thought to be a
ready remedy, the issue persists. The question facing healthcare providers today is, how can they leverage health IT to close these loops? (See “Closing the Loop: Considerations for How EHRs Can Help” on page 20.)
Failures to close the loop are multifactorial and range from a test not being performed at all, to a test not performed as ordered, to the results not
being returned to the clinician, to the clinician failing to acknowledge those results. Each of these chains of events creates a loop with the potential for a break, with the patient being central to all the loops involving diagnostic testing (e.g., provider to provider, provider to patient or caregiver, facility to provider). Any failure to close these loops holds the potential for patient harm through delayed, missed, or incorrect diagnoses.
MISSED DIAGNOSIS
A routine mammography was ordered.The patient failed to have the test performed, but continued with her routine visits.
Five years later, another routine mammogram was ordered for the patient. The results indicated a breast lump with infiltrating ductal carcinoma.
Unfortunately, a chart review uncovered a note from five years earlier, stating,"Mammo pending; no result." This indicates the patient was never followed up with, and thus the breast lump went undetected for five years.
In 2017, the Emergency Care Research Institute (ECRI) Partnership for Health IT Patient Safety convened the Closing the Loop Workgroup, chaired by Dr. Christoph U. Lehman. The workgroup was comprised of health IT vendors, clinicians, healthcare organizations, malpractices insurers,patient advocates, and representatives from professional organizations and societies, and held a goal to develop health IT safe practices for closing the loop to mitigate delayed, missed, and incorrect diagnoses.
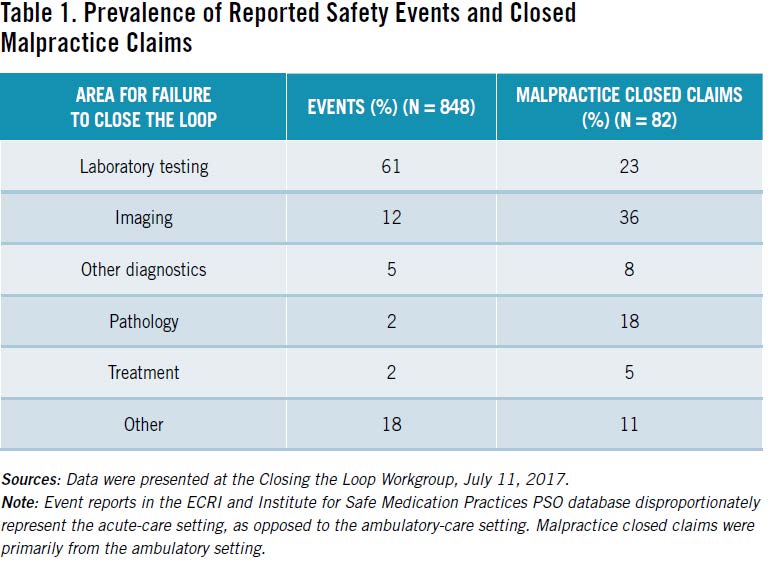
ECRI and the Institute for Safe Medication Practices’ PSO analyst reviewed more than 800 relevant events from the PSO database and performed
an additional review of more than 80 medical malpractice closed-claims reports. The analysis revealed that failure to close the loop on diagnostic
testing is primarily seen with six types of information (Table 1). The most common failures for safety events occurred in laboratory testing (61%),
followed by events related to imaging(12%). Data from closed medical malpractice claims suggest that imaging was the information most likely
to not be communicated (at 36%),followed by laboratory testing (23%) and pathology (18%).
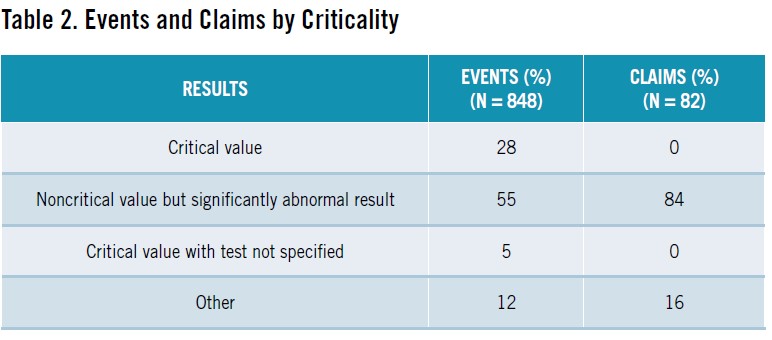
A critical result is defined as a result from a test that must be reported immediately
to a care provider, because it may require urgent therapeutic action. (See “Critical
Results Testing” on page 34.) Using this definition, we also grouped information
that was not communicated by criticality. Both for events and malpractice claims,
significantly abnormal noncritical results were more likely to not be communicated
(see Table 2).
Most failures to close the loop had multiple targets for notification. In reported safety events, staff were the most common target of communication (at 65%),followed by physicians (62%). However, for claims, the most common target was the physician (89%), followed by the patient (71%) and staff (46%).
Not surprisingly, only 19% of reported events resulted in a delay in treatment or diagnosis, while 96% of malpractice claims included a claim of delay in diagnosis or treatment. In the case of events, this delay was triggered mostly by failure to report or communicate (80%) and lag in reporting or awareness (19%). For claims, the most common reason was that a provider acknowledged information and failed to follow up (39%), followed by failure to report or communicate (30%), delay in reporting (21%), and unclear/ambiguous communication (16%).
DIAGNOSIS NOT COMMUNICATED
A patient admitted with shortness of breath was diagnosed with pneumonia.The radiology study identified a lung lesion; however, these findings were not communicated to the patient. There was no documentation of a follow-up or workup related to the lung lesion. The patient was admitted to the hospital six months later, and was diagnosed with an adenocarcinoma.
Eliminating diagnostic error requires closing the loop on diagnostic results—adding a plethora of technology alerts and reminders to an already
dysfunctional process for result management will only obfuscate matters.
The Closing the Loop Workgroup offers the following three recommendations for communicating, tracking, and linking, along with references and tools to facilitate their implementation:
SAFE-PRACTICE RECOMMENDATIONS
• Develop and apply information technology (IT) solutions to communicate the right information (including data needed for
interpretation) to the right people, at the right time, in the right format
• Implement IT solutions to track key areas
• Use health IT to link and acknowledge the review of information and documentation of the action taken
Communicate
The recommendation to communicate encourages stakeholders to design, test, deploy, and implement health IT solutions that improve communication pathways and make closing the loop a seamless and elegant process, with all diagnostic tests communicated to the provider, the pharmacy, and the patient in a timely manner.
The lack of standardization in healthcare creates a dangerous inconsistency across systems. One basic requirement for effective
communication is the use of standard nomenclature and structured data (e.g., SNOMED CT, LOINC) to improve the overall efficiency and usability of transmitted test results for reporting diagnoses. Today, providers work in multiple electronic health records (EHRs) as they move from the inpatient,ambulatory-care, and surgical centers. Information contained in records in these various settings is not often kept in the same location, formatted the same, or readily retrievable; this compromises safety, timely information gathering, and readiness to action. Well thought-out and agreed-upon standards can help reduce the cognitive workload of physicians.
To ensure successful communication, functionality must be available to generate reminders and disperse information as needed. This functionality may require providers and provider organizations to reevaluate their systems to ensure that all systems are working as intended. EHRs and clinical workflows must align to ensure that work is being performed as intended. Adopting and implementing standard nomenclature and terminology,display icons, and reporting criteria—including the timing and results priority for reporting findings—will make the process of closing the loop more efficient and effective. Finally, to guarantee closed-loop communication,it is essential to notify the patient of test results, including the follow-up plan, treatment, or therapy. The loop begins and ends with the patient.
Track
It is essential to implement health IT solutions to track key areas in the results-management process. Providers, healthcare organizations, and leadership all need to know when a loop remains open. Accurate tracking and monitoring of diagnostic results—including occurrence, transmission of information, acknowledgment,documentation, and responses—are essential to identify closed loops.
The safe-practice recommendation suggests that tracking and monitoring of test results is critical to identify interruptions and potential failure points in the process, including the ability to react to and remedy failures to close the loop. Results that do not reach the intended recipient, or that are not reviewed or acted upon, delay diagnosis and treatment and lead to diagnostic error. Similarly to the safe practice for communication,tracking calls for the use of standard nomenclature to automate the ordering and matching of results. Organizations should adopt all available methods offered by their EHR vendors to track results and identify breaks in the process such as incomplete orders, results not reviewed, missing acknowledgments by providers on critical results, results not transmitted to the patient, or results not viewed by the patient.
Although the intention is to make tracking an automated process, we can never completely remove the human element. Identifying potential failure
points through oversight and close monitoring of interface connectivity,error queues, and audit log review is essential, and automation of the process is improved using bidirectional communication with testing facilities,when available, and through standards such as LOINC, which improve the accuracy of matching diagnostic results in the patient record.
Link
The final safe-practice recommendations are to link and acknowledge. Linking and acknowledging advocates the development and use of health IT to ensure that all new information is reviewed and acted upon. The recommendation requires enlisting the support of developers and vendors to improve interoperability, including the use of application programming interfaces (APIs) to allow laboratory systems and hospital communication, as well as the use of HL7 and fast healthcare interoperability resources.The recommendation is a call to action for the development of functionality that can link an acknowledgement of results to the action taken; it aligns with the recommendations for improved interoperability outlined in the proposed rule on the 21st Century Cures Act implementation recently issued by the Office of the National Coordinator for Health IT.3
The ability of EHRs to exchange and make use of information within and across organizations must include functionality for acknowledgement and response.
AN ISSUE OF CONSEQUENCE
Closing the loop on diagnostic error is an issue of consequence in healthcare today. Providers face an increased burden in the present climate as they are challenged more and more to track test results, identify patients at risk, and share the information in a timely manner with patients, public-health departments, registries, and health information exchanges.
According to Sittig and Singh, more than one in every four adults will be impacted by a diagnosis error in their lifetime.4 Every year, healthcare costs related to diagnostic error continue to rise.5 According to a BMJ Quality & Safety article which analyzes U.S.malpractice claims for diagnosis errors,the 25-year sum (1986-2010) of diagnosis-related payment was $38.8 billion (https://qualitysafety.bmj.com/content/22/8/672).
By closing the loop to reduce the number of diagnostic errors and ensure that timely treatment and therapies are implemented, we can improve these outcomes for patients everywhere.